Selective Serotonin Reuptake Inhibitors (SSRIs) are a common type of antidepressant used to treat depression and other mental health conditions. These medications work by increasing serotonin levels in the brain, helping to improve mood and emotional balance. While SSRIs offer many benefits, they also come with potential side effects that users should understand.
Mental health challenges affect millions—nearly 1 in 5 adults and 1 in 6 youth in the U.S. face these issues annually, according to the National Alliance on Mental Illness (NAMI). SSRIs remain a key treatment option for managing these conditions effectively.
Read More: Types of Therapy for Treating Depression
What are SSRIs?
SSRIs are often the first choice for treating depression and several other mental health conditions due to their effectiveness and lower risk of side effects. These medications work by boosting serotonin levels in the brain, a neurotransmitter linked to mood regulation.
Although the exact cause of depression remains unclear, experts agree that low serotonin levels contribute significantly to the condition. By increasing serotonin, SSRIs help restore emotional balance and improve symptoms for many individuals.
Prescribing SSRIs: What they help treat
SSRIs are commonly prescribed for depression but are also effective for other conditions such as obsessive-compulsive disorder (OCD), generalized anxiety disorder, panic disorder, bulimia, bipolar depression, post-traumatic stress disorder (PTSD), premenstrual dysphoric disorder (PMDD), and general anxiety.
Additionally, SSRIs have several off-label uses, meaning they treat conditions beyond their original purpose. These include fibromyalgia, binge eating disorder, body dysmorphic disorder, and autism. Doctors may recommend SSRIs for these off-label cases based on their potential benefits and individual patient needs.
How SSRIs work
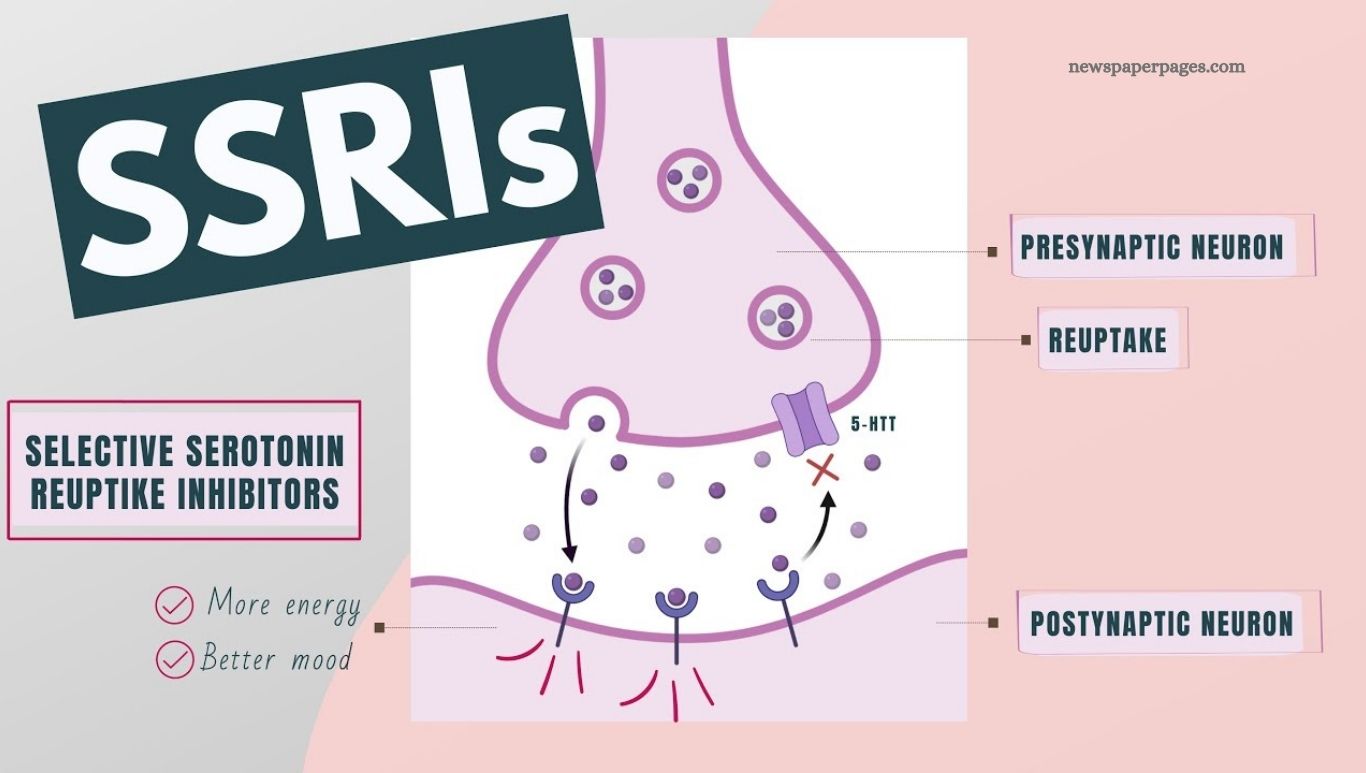
Serotonin is a key brain chemical that helps transmit signals between nerve cells and is often called the “feel-good chemical” for promoting a sense of well-being. Depression is linked to low levels of serotonin, along with other chemicals like dopamine and norepinephrine.
SSRIs work by blocking the absorption of serotonin into the bloodstream, increasing its availability in the brain. This boost helps ease depression symptoms. Unlike creating more serotonin, SSRIs improve how the body uses existing levels. While SSRIs share similar effectiveness, they differ in specific uses, side effects, and dosages.
SSRI drugs
Several SSRIs are available today, including:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac, Sarafem)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil, Paxil CR, Pexeva)
- Sertraline (Zoloft)
- Vilazodone (Viibryd)
Each medication has unique features but works similarly to increase serotonin levels and improve mood.
Possible side effects
SSRIs primarily target serotonin, causing fewer side effects than older antidepressants like tricyclics (TCAs) and monoamine oxidase inhibitors (MAOIs), which affect multiple brain chemicals. However, SSRIs can still cause side effects such as lowered libido, sleep disturbances, weight changes, anxiety, dizziness, dry mouth, headaches, and gastrointestinal issues.
The FDA warns that SSRIs may increase the risk of suicidal thoughts in children and young adults. Since depression itself can heighten this risk, it’s crucial to discuss these concerns with your doctor to carefully weigh the benefits and risks before starting treatment.
SSRI risks
“Selective serotonin reuptake inhibitors are generally very safe,” says Dr. Danny Carlat, associate clinical professor of psychiatry at Tufts University School of Medicine. He notes that while minor side effects may occur, it is unlikely for individuals to cause serious harm by taking an SSRI. However, caution is advised for certain groups, including children and pregnant individuals, who may require closer monitoring when using these medications.
For children
Research on SSRIs in children is limited, so younger patients should be closely monitored for mood or behavior changes during treatment.
For pregnant people
SSRIs may raise the risk of fetal developmental issues, particularly heart and lung problems. Doctors and expecting mothers must weigh the risks of SSRI use against untreated depression, which can also negatively affect pregnancy. Some may switch to SSRIs with fewer risks—paroxetine (Paxil), for example, is linked to fetal heart problems, so doctors might recommend alternatives like fluoxetine (Prozac) or citalopram (Celexa).
General risks
Inform your doctor about any existing health conditions such as epilepsy, diabetes, or kidney disease, as these may require closer monitoring. SSRIs can interact with other medications and supplements like St. John’s wort. Always disclose all prescription, over-the-counter drugs, and supplements to your healthcare provider.
When to consider taking SSRIs
Antidepressants like SSRIs can help relieve depression symptoms but usually work best as part of a broader treatment plan. Your doctor may also suggest therapy, which can offer tailored strategies based on your symptoms and personal history.
SNRIs vs. SSRIs
Serotonin-norepinephrine reuptake inhibitors (SNRIs) work like SSRIs by preventing the brain from reabsorbing too much serotonin, but they also block the reuptake of norepinephrine. This dual action makes SNRIs effective for treating depression, certain anxiety disorders, and nerve pain. Common SNRIs include venlafaxine (Effexor XR), desvenlafaxine (Khedezla, Pristiq), duloxetine (Irenka, Cymbalta), and milnacipran (Savella). Your doctor will help determine whether an SNRI or SSRI is the best treatment based on your specific symptoms and health conditions.
Can you drink alcohol on SSRIs?
Many doctors recommend avoiding alcohol while taking SSRIs because both can affect your mood and cause drowsiness or reduced alertness. Regular heavy drinking may also interfere with how well SSRIs work. However, since completely stopping alcohol can be challenging, moderate drinking is generally considered acceptable—about one drink per day, such as 12 oz. of beer, 5 oz. of wine, or 1 oz. of liquor. Always consult your doctor for personalized advice on alcohol use during SSRI treatment to ensure safety and effectiveness.
Frequently Asked Questions
What are SSRIs?
SSRIs are antidepressant medications that increase serotonin levels in the brain to help improve mood and relieve symptoms of depression and anxiety.
What conditions do SSRIs treat?
They are mainly used for depression, anxiety disorders, OCD, PTSD, panic disorder, and some off-label uses like fibromyalgia and binge eating disorder.
How long does it take for SSRIs to work?
It usually takes 4 to 6 weeks to notice significant improvement, though some effects may appear sooner.
What are common side effects?
Side effects can include nausea, headache, sleep disturbances, sexual issues, weight changes, and anxiety.
Can I drink alcohol while taking SSRIs?
Moderate alcohol use may be okay, but it’s best to discuss this with your doctor since alcohol can interfere with the medication.
Are SSRIs safe during pregnancy?
Some SSRIs carry risks during pregnancy; it’s important to weigh the benefits and risks with your healthcare provider.
Can SSRIs cause withdrawal symptoms?
Stopping SSRIs abruptly can lead to withdrawal symptoms, so always consult your doctor before changing your dosage.
Conclusion
Selective Serotonin Reuptake Inhibitors (SSRIs) play a vital role in treating depression and various mental health conditions by helping balance serotonin levels in the brain. While generally safe and effective, understanding their benefits, potential side effects, and interactions is essential for making informed decisions.
Always work closely with your healthcare provider to choose the right medication and treatment plan tailored to your needs. With proper guidance and monitoring, SSRIs can significantly improve quality of life and support mental health recovery.